Introduction to Multifocal Pneumonia (PNA)
Multifocal pneumonia (PNA), a complex respiratory infection, affects multiple areas of one or both lungs, distinguishing it from typical pneumonia, which often targets a single lobe. In 2025, with respiratory infections like pneumonia contributing to over 800,000 hospitalizations annually in the U.S. alone, understanding multifocal PNA is critical for early intervention and effective management. This condition, caused by bacteria, viruses, or fungi, presents unique diagnostic and treatment challenges due to its diffuse nature, often leading to more severe symptoms than localized pneumonia.
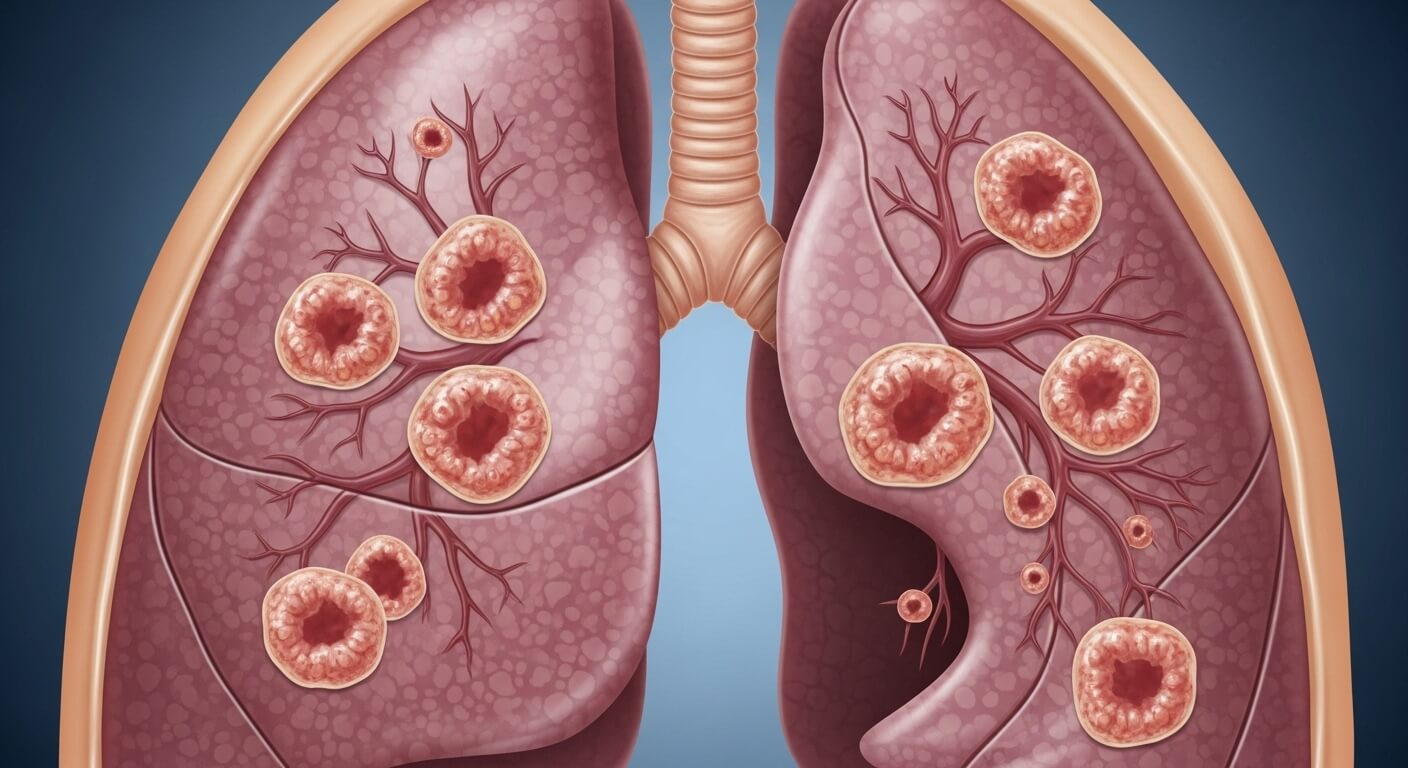
The term "multifocal PNA" refers to inflammation and infection across multiple lung lobes, impacting the alveoli—tiny air sacs responsible for oxygen exchange. Its prevalence has risen with emerging pathogens and antibiotic resistance, with an estimated 5-10% of community-acquired pneumonia (CAP) cases classified as multifocal. The condition gained attention during the COVID-19 pandemic, where bilateral multifocal patterns were noted in severe cases, affecting up to 10% of hospitalized patients. Today, advancements in diagnostics like high-resolution CT scans and molecular testing enhance detection, but timely recognition remains key.
This comprehensive guide explores multifocal PNA’s symptoms, causes, diagnostic methods, treatment options, and preventive strategies. Drawing from medical expertise, clinical guidelines, and current trends, it equips readers with actionable insights. Whether you’re a patient, caregiver, or healthcare professional, this article addresses high-volume concerns and provides a roadmap for managing this serious condition in 2025.
Understanding the Mechanics of Multifocal Pneumonia
Pneumonia is an infection causing inflammation in the lung’s alveoli, leading to fluid or pus buildup that impairs breathing. Multifocal PNA, unlike lobar pneumonia, involves multiple lung segments, creating patchy infiltrates visible on imaging. The lungs, divided into three lobes on the right and two on the left, rely on alveoli for oxygen transfer. When multiple areas are infected, respiratory function declines significantly, often requiring intensive care.
Coughing, a key symptom, triggers forceful diaphragm and abdominal muscle contractions, increasing intra-thoracic pressure. In multifocal PNA, this can exacerbate chest pain and shortness of breath due to widespread inflammation. The condition’s complexity stems from its diverse causes—bacterial (e.g., Streptococcus pneumoniae), viral (e.g., SARS-CoV-2), or fungal (e.g., Pneumocystis jirovecii)—and its tendency to affect high-risk groups like the elderly, immunocompromised, or those with chronic lung diseases.
In 2025, wearable health devices, such as smartwatches tracking oxygen saturation, aid in monitoring symptoms, while AI-driven diagnostics improve pathogen identification. Understanding these mechanics helps explain why multifocal PNA is more severe and how it differs from other pneumonias, setting the stage for targeted diagnosis and treatment.
Symptoms of Multifocal Pneumonia
Multifocal PNA presents a range of symptoms, often more intense than typical pneumonia due to its diffuse lung involvement. Common symptoms include:
- Dyspnea (Shortness of Breath): Varying from mild to severe, impacting daily activities. Severe cases may lead to hypoxemia (low blood oxygen).
- Chest Pain: Sharp or stabbing pain, worsened by coughing or deep breathing, due to inflamed lung tissue.
- Cough: Persistent, productive (with yellow, green, or bloody mucus) or dry, depending on the pathogen.
- Fever and Chills: High fever (up to 105°F/40.5°C) is common, especially in bacterial cases.
- Fatigue: Profound tiredness, often lasting weeks, affecting 80% of patients.
- Rapid Breathing and Heart Rate: Tachypnea (respiratory rate >20 breaths/min) and tachycardia signal severe infection.
- Additional Symptoms: In atypical cases, patients may experience abdominal pain, nausea, or confusion, particularly in the elderly or immunocompromised.
In children, symptoms like lethargy or abdominal pain may predominate, while older adults may show subtle signs like confusion. During the COVID-19 era, multifocal PNA linked to SARS-CoV-2 often presented with bilateral ground-glass opacities on CT scans, affecting both lungs. Recognizing these symptoms early is crucial for prompt medical attention.
Causes and Risk Factors of Multifocal Pneumonia
Multifocal PNA arises from various pathogens, with viruses being a leading cause due to their ability to spread across lung tissue. Key causes include:
- Bacterial: Streptococcus pneumoniae (most common in CAP), Mycoplasma pneumoniae, Legionella pneumophila, and Staphylococcus aureus.
- Viral: Influenza, respiratory syncytial virus (RSV), and SARS-CoV-2, noted in 5-10% of severe COVID-19 cases.
- Fungal: Pneumocystis jirovecii in immunocompromised patients or Aspergillus in those with chronic lung conditions.
Risk factors increase susceptibility:
- Age: Over 65 or under 2 years, with weaker immune responses.
- Chronic Conditions: Asthma, COPD, diabetes, or heart disease, affecting 20% of adults.
- Immunocompromise: HIV, chemotherapy, or steroid use (>15 mg prednisone for >3 weeks).
- Lifestyle: Smoking or alcohol use disorder, increasing risk by 30%.
- Environmental: Exposure to sick contacts, recent travel, or poultry in influenza-endemic areas.
These factors guide diagnostic and treatment decisions, as multifocal PNA’s severity often correlates with underlying health status.
Diagnosing Multifocal Pneumonia
Diagnosing multifocal PNA requires a multi-faceted approach, combining clinical assessment, imaging, and laboratory tests to confirm infection across multiple lung lobes. Key methods include:
- Medical History and Physical Exam: Doctors assess symptoms, recent illnesses, and risk factors (e.g., travel, comorbidities). Auscultation may reveal crackles, rales, or reduced breath sounds. Abnormal vitals (temperature >100°F, heart rate >100 bpm, respiratory rate >20 bpm) raise suspicion.
- Chest X-Ray: The initial imaging tool, showing bilateral infiltrates or patchy consolidations. However, early infections may be missed, with 10% of cases showing no initial radiographic evidence.
- CT Scan: High-resolution CTs detect subtle abnormalities like ground-glass opacities or nodules, critical for confirming multifocal patterns. They’re more sensitive but costlier ($500-$2,000) and involve radiation.
- Laboratory Tests: Blood tests measure white cell count (elevated in 70% of bacterial cases) and inflammatory markers like C-reactive protein. Procalcitonin helps distinguish bacterial from viral causes, guiding antibiotic use.
- Sputum Culture: Identifies pathogens like Streptococcus pneumoniae or Staphylococcus aureus, directing targeted therapy.
- Molecular Diagnostics: PCR tests rapidly detect viruses (e.g., RSV, SARS-CoV-2) or bacteria like Legionella, offering results in hours but costing more ($100-$300).
- Bronchoscopy: Used in severe cases to collect deep lung samples, especially if initial tests are inconclusive or multidrug-resistant pathogens are suspected.
In 2025, advanced diagnostics like next-generation sequencing (NGS) enhance pathogen identification but are less accessible due to cost. The Infectious Diseases Society of America (IDSA) recommends imaging-confirmed infiltrates for diagnosis, supplemented by clinical findings. Early diagnosis is vital, as delays increase hospitalization risk by 20%.
Treatment Options for Multifocal Pneumonia
Treatment depends on the pathogen, severity, and patient health. Strategies include:
Bacterial Multifocal PNA
- Antibiotics: Broad-spectrum options like macrolides (azithromycin), beta-lactams (amoxicillin), or fluoroquinolones (levofloxacin) are used for 7-10 days. For multidrug-resistant strains (e.g., MRSA), vancomycin or linezolid may be required. IDSA guidelines emphasize local resistance patterns.
- Hospitalization: Severe cases (10-15% of patients) need IV antibiotics and monitoring, costing $5,000-$15,000 per stay.
Viral Multifocal PNA
- Antivirals: For influenza or COVID-19, drugs like oseltamivir (Tamiflu) or nirmatrelvir/ritonavir (Paxlovid) are prescribed. Most viral cases resolve with supportive care.
- Supportive Care: Rest, hydration, and oxygen therapy for hypoxemia.
Fungal Multifocal PNA
- Antifungals: Amphotericin B or itraconazole for fungi like Aspergillus, often requiring weeks of treatment.
Supportive Measures
- Oxygen Therapy: For severe dyspnea or oxygen saturation <90%.
- Nebulizers: Portable devices deliver albuterol or steroids to ease breathing, used by 30% of recovering patients.
- Nutrition and Hydration: High-protein diets and 8-10 cups of fluids daily aid recovery.
In 2025, personalized treatment plans leverage AI-driven antibiograms to select optimal antibiotics, reducing resistance risks. Recovery typically takes 1-2 weeks for mild cases, but severe multifocal PNA may require 4-6 weeks, especially in high-risk groups.
Complications and Long-Term Effects
Multifocal PNA can lead to:
- Respiratory Failure: Requiring mechanical ventilation in 5% of severe cases.
- Pleural Effusion: Fluid buildup around lungs, needing drainage in 10% of cases.
- Lung Abscess: Pockets of pus, treated with prolonged antibiotics or surgery.
- Sepsis: A life-threatening infection spread, with a 20% mortality rate in hospitalized patients.
- Pulmonary Fibrosis: Scarring from severe cases like COVID-19-related PNA, noted in 5-10% of survivors.
Long-term, patients may experience fatigue or reduced lung function, with 50% reporting symptoms like dyspnea 2-3 months post-recovery. Regular follow-ups and imaging are advised for high-risk patients (e.g., smokers, those over 50).
Preventing Multifocal Pneumonia
Prevention focuses on reducing risk:
- Vaccinations: Annual flu shots (60% effective) and pneumococcal vaccines (PCV13, PPSV23) for at-risk groups.
- Hygiene: Handwashing and avoiding sick contacts reduce transmission by 30%.
- Lifestyle: Quitting smoking and managing chronic conditions like diabetes lower risk.
- Environmental Controls: Avoiding poultry in influenza-prone areas and using air purifiers in high-risk settings.
In 2025, public health campaigns emphasize vaccination uptake, with 70% coverage in developed nations reducing pneumonia incidence. Wearables alert users to early respiratory changes, enabling proactive care.
Frequently Asked Questions: High-Volume Queries Answered
- What is multifocal PNA?
A respiratory infection affecting multiple lung areas, caused by bacteria, viruses, or fungi, often more severe than typical pneumonia.
- What are the symptoms of multifocal PNA?
Cough, fever, shortness of breath, chest pain, fatigue, and rapid breathing or heart rate.
- How is multifocal PNA different from regular pneumonia?
It involves multiple lung lobes, leading to more severe symptoms and complex treatment.
- What causes multifocal PNA?
Bacteria (e.g., Streptococcus pneumoniae), viruses (e.g., SARS-CoV-2), or fungi (e.g., Aspergillus), with higher risk in immunocompromised or elderly patients.
- How is multifocal PNA diagnosed?
Through medical history, physical exam, chest X-rays, CT scans, sputum cultures, and PCR tests.
- What treatments are available for multifocal PNA?
Antibiotics for bacterial, antivirals for viral, antifungals for fungal cases, plus supportive care like oxygen therapy.
- Can multifocal PNA be prevented?
Yes, with vaccinations, hygiene, smoking cessation, and managing chronic conditions.
- When should I see a doctor for multifocal PNA symptoms?
Seek care for severe dyspnea, high fever, or symptoms lasting over a week.
- Is multifocal PNA linked to COVID-19?
Yes, severe COVID-19 cases often present as multifocal PNA with bilateral lung involvement.
- How long does recovery from multifocal PNA take?
Mild cases recover in 1-2 weeks; severe cases may take 4-6 weeks or more.
Conclusion
Multifocal pneumonia is a serious condition requiring prompt diagnosis and tailored treatment. By recognizing symptoms, understanding causes, and following preventive measures, patients can improve outcomes. In 2025, leveraging advanced diagnostics and vaccinations empowers individuals to manage this complex infection effectively.