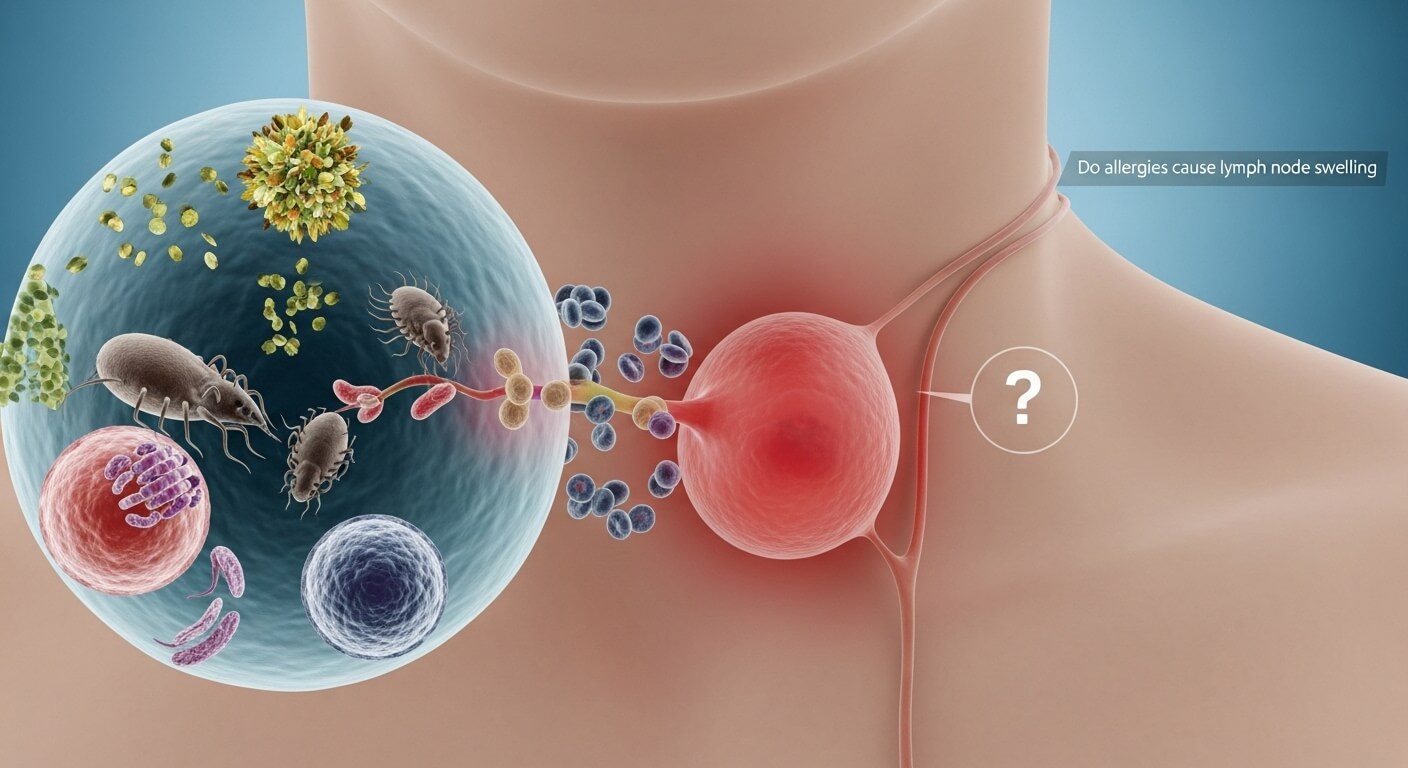
Lymph node swelling, or lymphadenopathy, is a common concern that raises questions about its causes, especially for those experiencing allergies. A frequent query is: do allergies cause lymph node swelling? Typically, allergies like hay fever or mild food sensitivities do not directly cause lymph node swelling, but they can contribute indirectly by triggering conditions like infections or severe inflammation. This comprehensive article explores the relationship between allergies and lymph nodes, covering causes, symptoms, diagnosis, treatments, prevention strategies, and answers to common questions. Grounded in medical insights as of 2025, this guide offers clear, actionable information to help you understand and manage this condition effectively.
What Are Allergies?
Allergies occur when the immune system overreacts to harmless substances, known as allergens, such as pollen, dust mites, pet dander, mold, or certain foods. When exposed to these triggers, the body releases chemicals like histamine, causing inflammation and symptoms to expel the perceived threat. Common allergy types include seasonal allergies (hay fever or allergic rhinitis), food allergies, skin allergies (eczema or hives), and insect sting allergies.
Allergic reactions can range from mild (sneezing, itchy eyes) to severe (anaphylaxis, a life-threatening response). Allergies affect over 50 million Americans annually, with symptoms often worsening in spring or fall due to high pollen counts. The immune system produces antibodies (IgE) that bind to allergens, activating mast cells and basophils to release inflammatory mediators.
While allergies typically affect the respiratory system, skin, or digestive tract, their systemic effects can occasionally extend to other areas, including the lymphatic system. However, the connection to lymph node swelling is not straightforward, as we’ll explore.
What Are Lymph Nodes and Lymph Node Swelling?
Lymph nodes are small, bean-shaped structures within the lymphatic system, which helps fight infections and maintain fluid balance. Hundreds of nodes are located in areas like the neck, armpits, groin, and abdomen, acting as filters that trap viruses, bacteria, and other foreign substances, where immune cells (lymphocytes) neutralize them.
Lymph node swelling occurs when nodes enlarge due to increased immune activity, often from infection, inflammation, or cancer. Normal nodes are pea-sized and painless; swollen ones can be tender, firm, or rubbery, ranging from marble-sized to larger. Swelling may be localized (one area) or generalized (multiple areas) and can last days to weeks.
Common causes include viral infections (like colds or mononucleosis), bacterial infections (strep throat), autoimmune diseases (rheumatoid arthritis), or malignancies (lymphoma). Environmental factors or medications can also contribute. In 2025, with growing awareness of post-viral syndromes, swollen nodes are increasingly linked to immune dysregulation.
Understanding lymph nodes is essential because swelling signals an immune response, which may be benign or serious. Now, let’s address the link to allergies.
Do Allergies Cause Lymph Node Swelling?
In most cases, typical allergies like seasonal hay fever or mild food sensitivities do not directly cause lymph node swelling. Lymph nodes enlarge primarily in response to infections, where pathogens multiply and trigger a strong immune response. Allergies involve a type I hypersensitivity reaction focused on histamine release, leading to symptoms like itching or sneezing, but not typically lymph node enlargement.
However, there are exceptions and indirect connections. Severe allergic reactions, such as anaphylaxis, or chronic allergic conditions can lead to inflammation that indirectly affects lymph nodes. For example, allergies can cause sinusitis or ear infections, which then trigger swollen nodes in the neck or jaw area. In rare cases, extreme allergen exposure (e.g., heavy pollen or severe food allergies) might cause mild, temporary node swelling due to an intense immune response.
Medical sources emphasize that allergies are more likely to contribute to swelling through secondary complications. Allergic rhinitis, for instance, can cause postnasal drip, fostering bacterial growth and infection, which then swells nodes. In 2025, with increased pollen counts due to climate change, such indirect effects are more prevalent, affecting up to 20% of allergy sufferers with secondary symptoms.
If lymph nodes swell during allergy season without infection signs (fever, pus), it may be coincidental or due to another cause. Always consult a doctor to rule out serious conditions.
Mechanisms: How Allergies Might Indirectly Cause Lymph Node Swelling
While direct causation is rare, several mechanisms explain how allergies might indirectly lead to lymph node swelling:
- Secondary Infections: Allergies cause mucus buildup in the sinuses or throat, creating an environment for bacteria or viruses to thrive, which then activates lymph nodes.
- Inflammatory Response: Severe allergies release cytokines and other mediators, causing systemic inflammation that may mildly enlarge nodes, especially in the neck or groin.
- Immune Overactivation: Chronic allergies can lead to hypersensitivity, where the lymphatic system overreacts, similar to autoimmune conditions.
- Allergic Reactions to Medications: Some allergy treatments, like antibiotics for misdiagnosed infections, can cause drug reactions leading to node swelling.
- Environmental Allergens: Mold or dust allergies can mimic infections, indirectly causing node swelling through prolonged exposure.
These pathways show why allergies alone aren’t typically the cause but can exacerbate underlying issues.
Symptoms of Lymph Node Swelling Potentially Related to Allergies
If allergies contribute to lymph node swelling, symptoms often align with typical allergy signs:
- Tender or Painful Nodes: Swelling in the neck, under the jaw, or behind the ears; nodes feel soft and movable.
- Accompanying Allergy Symptoms: Sneezing, runny nose, itchy eyes, hives, or coughing.
- Fatigue and Malaise: General tiredness from immune activity.
- Fever or Chills: If a secondary infection develops.
- Skin Reactions: Rashes or redness near swollen areas.
- Respiratory Issues: Wheezing or shortness of breath in asthma-allergy overlaps.
Swelling is usually bilateral (both sides) and resolves with allergy management. Persistent, painless, or hard nodes require immediate medical attention, as they could indicate non-allergic causes like lymphoma.
Other Causes of Lymph Node Swelling
To provide context, lymph node swelling has many causes beyond allergies:
- Infections: Viral (colds, flu), bacterial (strep throat), fungal.
- Autoimmune Diseases: Lupus, rheumatoid arthritis.
- Cancers: Lymphoma, leukemia, or metastatic cancer.
- Medications: Reactions to vaccines or drugs.
- Environmental Factors: Irritants like smoke.
Allergies rank low among these causes, but misdiagnosis can occur if allergy symptoms mask infections.
Diagnosis of Lymph Node Swelling Related to Allergies
Diagnosing lymph node swelling begins with a physical exam and a review of medical history. Doctors palpate nodes and ask about allergy exposure, symptom duration, and family history. Diagnostic steps include:
- Blood Tests: To check IgE levels, infection markers, or autoimmune indicators.
- Imaging: Ultrasound, CT, or MRI to assess node size and structure.
- Allergy Testing: Skin prick or blood tests to identify specific allergens.
- Biopsy: Rarely needed for persistent swelling to rule out cancer.
- ENT Evaluation: For sinus-related issues.
In 2025, at-home allergy tests and AI-assisted diagnostics streamline initial assessments, but professional confirmation is crucial.
Treatment Options for Lymph Node Swelling from Allergies
Treatment focuses on managing allergies and addressing any secondary causes:
Medical Treatments
- Antihistamines: Over-the-counter options like loratadine reduce inflammation.
- Decongestants: Relieve congestion-related swelling.
- Corticosteroids: Nasal sprays or oral steroids for severe cases.
- Immunotherapy: Allergy shots or sublingual tablets for long-term relief.
- Antibiotics: If a secondary infection is present.
Home Remedies
- Hydration and Rest: Support immune function.
- Warm Compresses: Soothe tender nodes.
- Allergen Avoidance: Use air purifiers, wash bedding frequently.
- Herbal Supplements: Quercetin or butterbur for natural antihistamine effects (consult a doctor first).
Monitor swelling and avoid self-diagnosis; persistent cases require professional evaluation.
Prevention of Lymph Node Swelling Related to Allergies
Preventive measures focus on controlling allergies:
- Identify Triggers: Through allergy testing.
- Environmental Controls: Use HEPA filters, hypoallergenic bedding.
- Lifestyle: Maintain a balanced diet and exercise to boost immunity.
- Medications: Take prophylactic antihistamines during high-allergen seasons.
- Vaccinations: Stay current with flu vaccines to prevent secondary infections.
Regular check-ups help detect issues early.
High-Volume Questions About Allergies and Lymph Node Swelling
1. Can seasonal allergies cause swollen lymph nodes?
Rarely directly, but they can lead to infections that cause swelling.
2. Do food allergies cause lymph node swelling?
Severe food reactions might contribute, but it’s uncommon; infections are more likely.
3. Can pet allergies cause swollen lymph nodes?
Indirectly, through chronic exposure leading to inflammation or infection.
4. What do allergy-related swollen lymph nodes feel like?
Tender, movable nodes accompanied by allergy symptoms like itching or sneezing.
5. Can mold allergies cause swollen glands?
Yes, mold can trigger strong responses or infections that swell nodes.
6. Do allergies cause swollen lymph nodes in the neck?
The neck is a common site if sinusitis or infections develop from allergies.
7. Can dust allergies lead to lymphadenopathy?
Through chronic irritation and secondary infections, yes.
8. What home remedies help swollen lymph nodes from allergies?
Warm compresses, hydration, and allergen avoidance can reduce symptoms.
9. When should I see a doctor for swollen lymph nodes with allergies?
If swelling lasts over two weeks, is painful, or includes fever, seek medical advice.
10. Can pollen allergies cause armpit lymph node swelling?
Unlikely; neck swelling is more common, but severe cases could affect other areas.
11. Do allergies cause swollen lymph nodes in the groin?
Rarely; groin swelling usually points to other causes.
12. Can allergic reactions to medications cause swollen lymph nodes?
Yes, drug allergies are a known cause of node swelling.
13. What tests diagnose allergy-related swollen lymph nodes?
Blood tests, imaging, and allergy panels identify the cause.
14. Can chronic allergies lead to persistent lymph node swelling?
Yes, if untreated, they can cause complications leading to prolonged swelling.
15. Do allergies cause swollen lymph nodes in children?
More common in children due to frequent infections, but careful monitoring is needed.
Conclusion
Allergies rarely cause direct lymph node swelling, but they can contribute indirectly through infections or intense inflammation. By understanding the symptoms, seeking timely diagnosis, and managing allergies proactively, you can reduce the risk of complications. If lymph node swelling persists or worsens, consult a healthcare professional to rule out serious conditions. With proper care, most cases resolve quickly, improving comfort and well-being.